Systemic Lupus Erythematosus (SLE) is a complex autoimmune disease known to impact multiple organs, including the skin, joints, kidneys, heart, and brain. While common symptoms include joint pain, skin rashes, and fatigue, neurological complications of SLE are among the most serious and challenging aspects of the disease. Understanding these neurological manifestations is crucial for both patients and healthcare providers.
What is Systemic Lupus Erythematosus (SLE)?
Systemic Lupus Erythematosus, often referred to simply as lupus, occurs when the body’s immune system mistakenly attacks its tissues, causing widespread inflammation and damage. The exact cause of SLE remains unknown, but a combination of genetic, environmental, and hormonal factors likely contribute to its development. This autoimmune condition predominantly affects women, particularly those of reproductive age, and can range from mild symptoms to life-threatening complications.
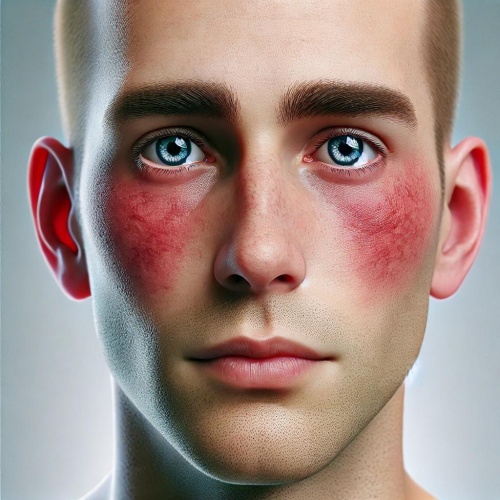
Common SLE symptoms include:
- Fatigue and joint pain
- Skin rashes, especially a butterfly-shaped rash over the cheeks
- Fever and kidney issues
However, one of the most challenging aspects of SLE for many patients is the neurological complications.
Neurological complications of Systemic Lupus Erythematosus (SLE)
Neurological involvement in SLE, known as Neuropsychiatric SLE (NPSLE), affects approximately 40-60% of individuals with lupus. These neurological symptoms can be diverse, impacting both the central and peripheral nervous systems. Here are some of the most common manifestations:
1. Central Nervous System (CNS) complications in SLE
The central nervous system is frequently affected by SLE, and complications can range widely:
- Chronic Headaches: Headaches, including migraines, are common among people with SLE. These can sometimes be secondary headaches due to inflammation, stress, or changes in cerebral blood flow.
- Cognitive Dysfunction in SLE: Often termed "lupus fog," cognitive dysfunction can affect memory, attention, and processing speed, complicating everyday tasks and decision-making.
- Seizures in Lupus: Around 10% of SLE patients experience seizures, likely due to inflammation or the presence of autoantibodies in the brain.
- Mood Disorders: Depression, anxiety, and mood swings are commonly reported among people with lupus and are often exacerbated by the chronic nature of the disease.
- Psychosis and Lupus: Although rare, psychosis can occur in SLE, manifesting as hallucinations or delusions. This requires immediate intervention for effective management.
- Cerebrovascular Disease and Stroke: People with lupus are at an increased risk of stroke due to factors like antiphospholipid syndrome, a condition that leads to abnormal blood clotting.
2. Peripheral Nervous System (PNS) complications in SLE
While less common than CNS involvement, peripheral nervous system complications can significantly impact quality of life:
- Peripheral neuropathy in Lupus: Damage to peripheral nerves can lead to pain, numbness, and tingling in the hands and feet, often due to inflammation.
- Cranial neuropathy and Lupus: Some individuals may experience cranial neuropathy, impacting vision or causing facial weakness.
- Myopathy and muscle weakness: Muscle inflammation in SLE can cause weakness, especially in larger muscle groups, potentially impacting mobility and daily activities.
Diagnosing neurological complications of SLE
Early and accurate diagnosis of neurological complications in SLE is crucial. Common diagnostic steps include:
- Neuroimaging: MRI or CT scans can reveal brain inflammation, blood vessel abnormalities, and ischemic lesions.
- Electroencephalography (EEG): EEG tests can identify abnormal electrical activity in the brain, which is especially helpful in diagnosing seizures.
- Cerebrospinal Fluid (CSF) Analysis: This test may show signs of CNS inflammation.
- Blood Tests: Specific antibodies such as anti-ribosomal P and anti-NMDA receptor antibodies can help confirm NPSLE diagnosis.
Treatment options for neurological complications in SLE
Managing neurological symptoms in lupus often requires a multidisciplinary approach, including both medications and lifestyle adjustments:
- Immunosuppressive medications: Drugs like corticosteroids, azathioprine, and mycophenolate mofetil are commonly used to reduce inflammation and prevent further nerve damage.
- Antimalarial drugs: Hydroxychloroquine, a key medication in SLE treatment, can also alleviate neuropsychiatric symptoms.
- Anticonvulsants and antipsychotics: For those experiencing seizures or psychosis, these medications help manage symptoms effectively.
- Psychotherapy and antidepressants: Cognitive therapy and antidepressant medications can help address mood disorders and cognitive impairment in lupus patients.
- Anticoagulants: For patients with antiphospholipid syndrome, anticoagulant therapy is essential to prevent stroke and other blood clot-related issues.
The Prognosis of neurological Involvement in SLE
While neurological complications in SLE can be severe, early diagnosis and prompt treatment can lead to better outcomes. Regular follow-ups with a rheumatologist and neurologist are essential to monitor disease activity and tailor treatment as needed. With comprehensive care, many people with SLE can successfully manage neurological symptoms and maintain a good quality of life.
Systemic Lupus Erythematosus (SLE) is a multifaceted autoimmune disease with significant neurological implications. By recognizing the signs of neurological involvement and seeking timely treatment, patients and healthcare providers can better manage this challenging aspect of lupus, improving long-term health and well-being.